A Nurse Practitioner SOAP Note Example is a valuable tool for nurse practitioners in documenting patient encounters and providing a comprehensive summary of assessments, diagnoses, treatments, and plans. It offers a structured format that ensures clear communication, consistency, and accuracy in documentation. Following the SOAP framework, nurse practitioners can effectively capture subjective and objective information, analyze the patient’s condition, and develop appropriate care plans. The example serves as a visual reference and learning tool, enabling nurse practitioners to enhance their documentation skills and deliver optimal patient care.
What Is a Nurse Practitioner SOAP Note?
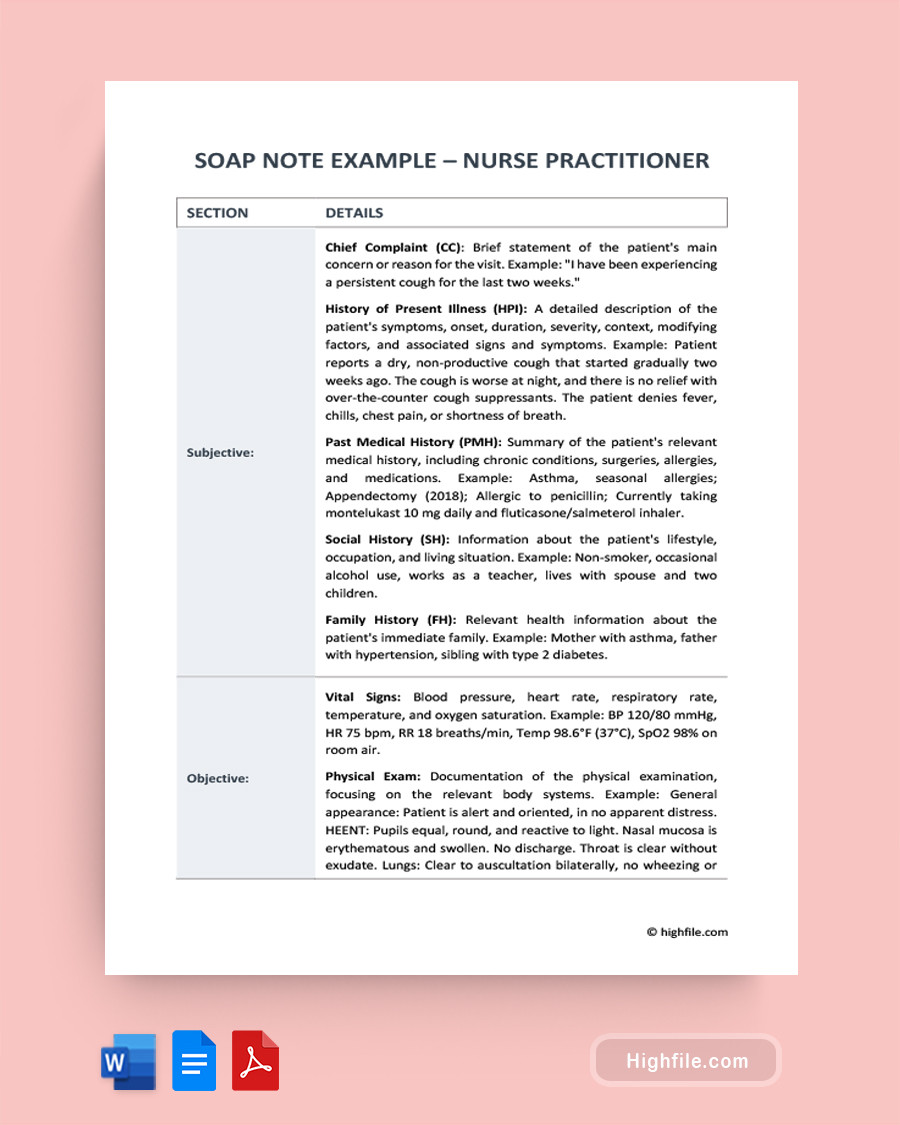
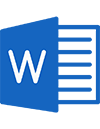
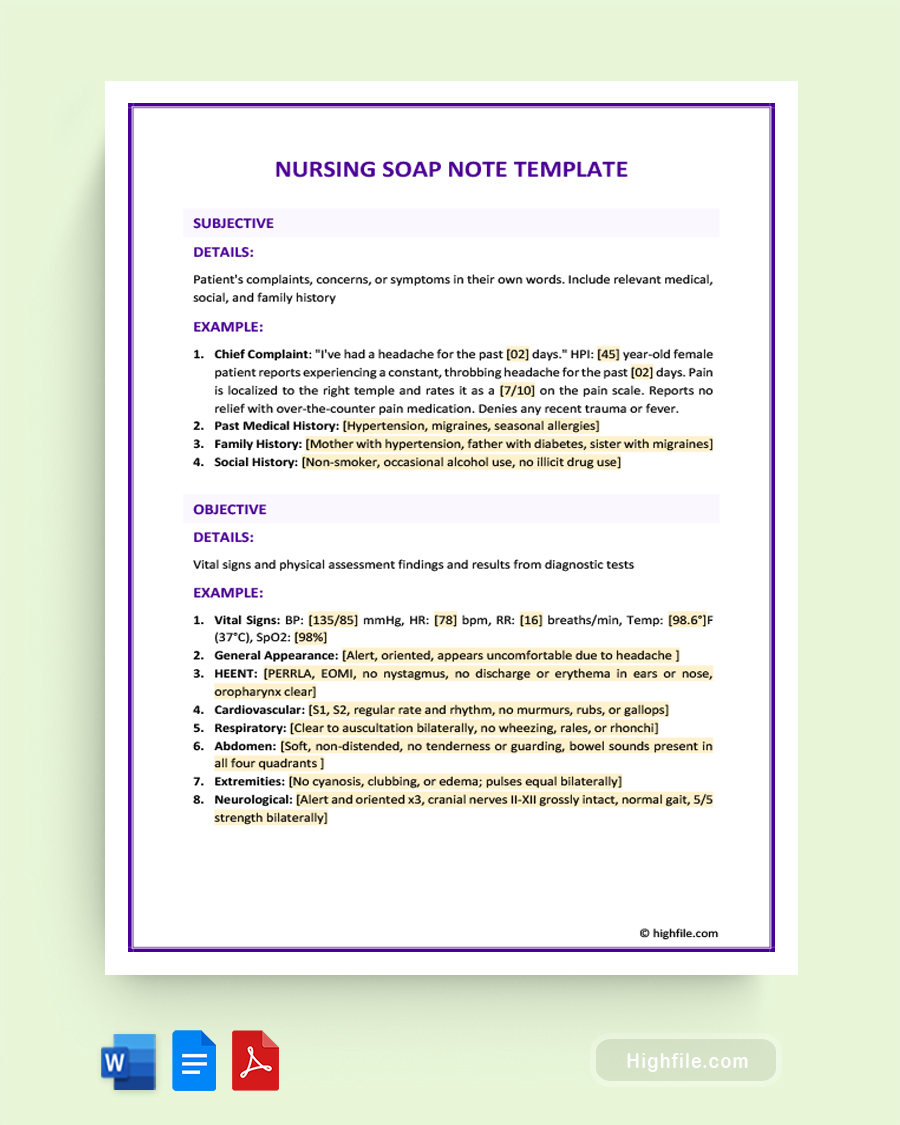
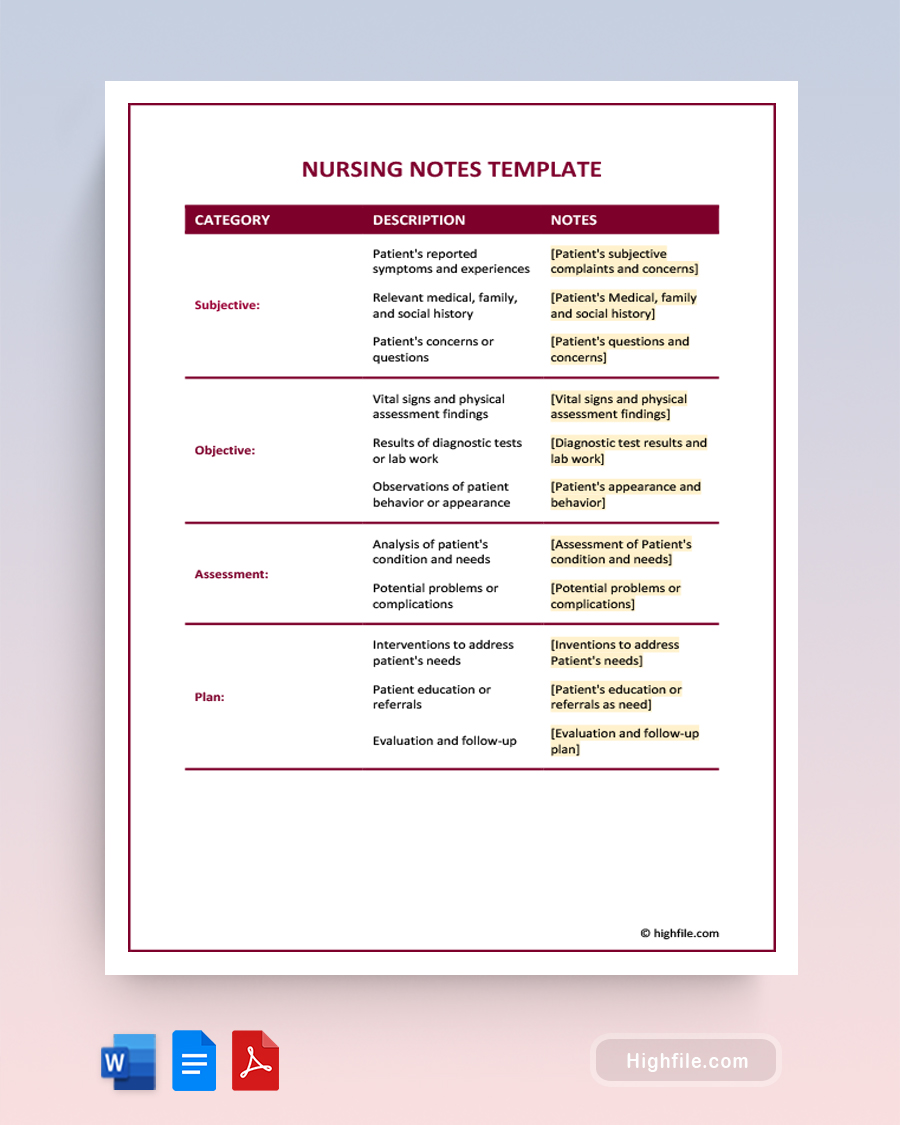
A Nurse Practitioner SOAP Note is a structured documentation format commonly used by nurse practitioners to record patient encounters and provide a comprehensive summary of the patient’s assessment, diagnosis, treatment, and follow-up plan. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, representing the four key components of the note. The Subjective section includes information gathered from the patient’s verbal account, such as symptoms and medical history. The Objective section consists of measurable data obtained through physical examination, diagnostic tests, and observations. The Assessment section includes the nurse practitioner’s professional analysis and diagnosis of the patient’s condition. Finally, the Plan section outlines the proposed treatment plan, including medications, therapies, referrals, and follow-up appointments.
Essential Elements of a Good Nurse Practitioner SOAP Note
A well-structured Nurse Practitioner SOAP Note is vital for effectively documenting patient encounters. It encompasses key sections that comprehensively overview the patient’s subjective information, objective findings, assessment, and plan. Here are the essential elements of a good Nurse Practitioner SOAP Note:
Subjective:
- Chief Complaint (CC): The patient’s main reason for seeking healthcare services.
- History of Present Illness (HPI): A detailed account of the current illness, including the onset, duration, severity, and associated symptoms.
- Past Medical History (PMH): Information about the patient’s previous medical conditions, surgeries, and significant medical events.
- Social History (SH): Details about the patient’s lifestyle, occupation, living environment, social support, and relevant habits (e.g., smoking, alcohol consumption).
- Family History (FH): Information about medical conditions that may have a genetic or familial component.
Objective:
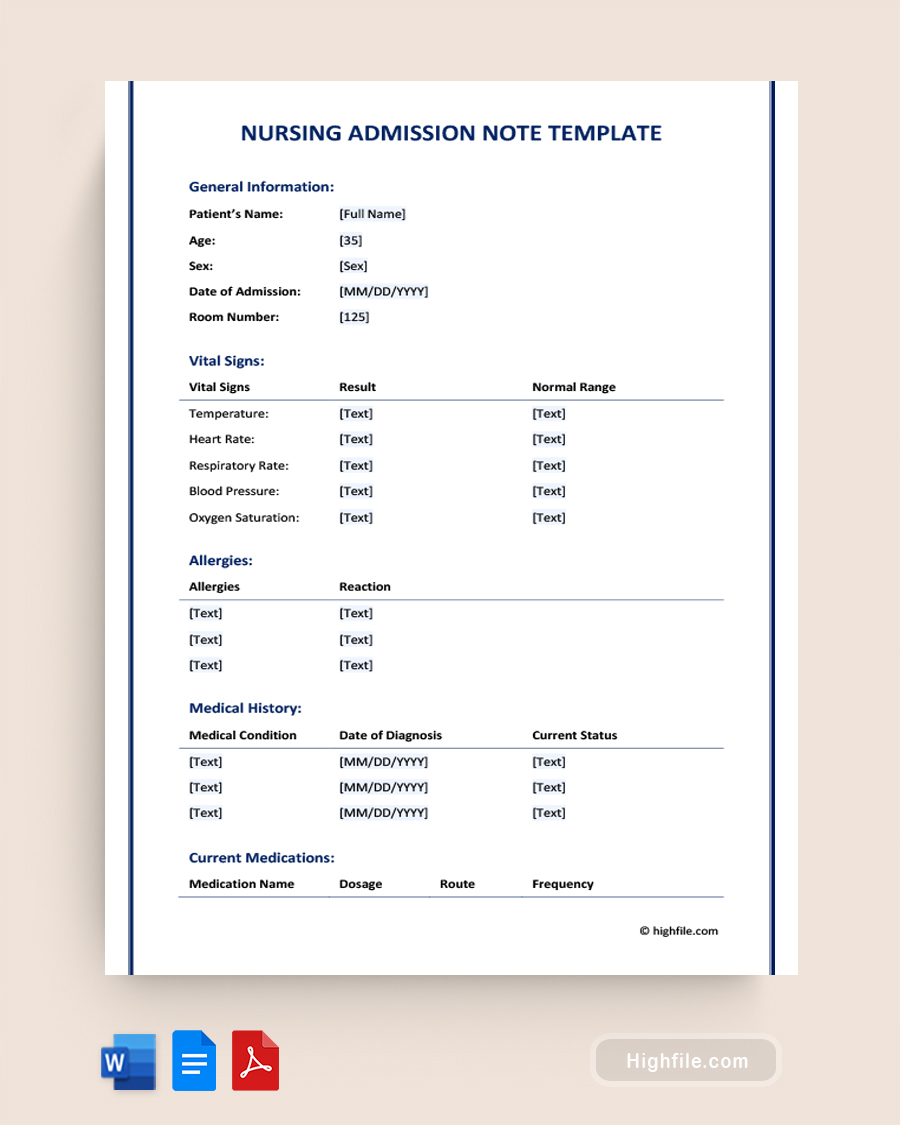
- Vital Signs: Recording measurements such as blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation.
- Physical Exam: Document findings from a systematic examination of the patient’s body systems, including general appearance, specific organ systems, and any abnormalities.
Assessment:
- Diagnosis/Problem List: The nurse practitioner’s professional analysis and identification of the patient’s health conditions or problems.
- Supporting Data: Any additional information or test results that support the diagnosis or problem list, such as laboratory values or imaging findings.
Plan:
- Diagnostic Tests: Specifying any further investigations or tests required to confirm or evaluate the patient’s condition.
- Treatment: Outlining the recommended interventions, including medications, therapies, procedures, or referrals to other healthcare providers.Patient Education: Document the education provided to the patient regarding their condition, treatment, self-care instructions, and follow-up plans.
Fun Fact: The SOAP note was developed by Dr. Lawrence Weed, an American physician and educator, in the 1960s. Dr. Weed introduced the concept as a standardized method of documenting patient encounters and organizing clinical information in a structured format. Dr. Weed’s innovation revolutionized medical documentation, providing a systematic approach that has been widely adopted in healthcare settings around the world.
How Can a Nurse Practitioner SOAP Note Example be Helpful?
A Nurse Practitioner SOAP Note Example can be helpful in the following ways:
- It provides a visual reference and learning tool for nurse practitioners to understand the structure and content of a well-crafted SOAP note.
- Demonstrates the appropriate language and terminology in documenting subjective and objective findings, promoting clear and concise communication.
- Serves as a template for capturing essential patient information systematically, ensuring comprehensive documentation, and reducing the risk of missing critical details.
- Enhances interdisciplinary communication by providing a standardized format that other healthcare professionals can easily understand and utilize.
- Facilitates efficient documentation by providing prompts and guidance, saving time and effort in creating well-structured SOAP notes.
FAQs
The length of each section in a SOAP note can vary depending on the complexity of the patient encounter and the specific documentation requirements of the healthcare setting. However, as a general guideline, an ideal length for each section is as follows:
ᐅ Subjective: The subjective section should be concise and focused, where the patient’s symptoms and medical history are recorded. Typically, it may range from a few sentences to a paragraph summarizing the patient’s relevant subjective information.
ᐅ Objective: The objective section, which includes the results of physical examinations, diagnostic tests, and observations, should be detailed and precise. It may span a few paragraphs, documenting the objective findings and measurable data collected during the encounter.
ᐅ Assessment: The assessment section, where the nurse practitioner analyzes and interprets the subjective and objective information, should be succinct but comprehensive. It may consist of one or two paragraphs summarizing the nurse practitioner’s professional analysis and diagnosis of the patient’s condition.
ᐅ Plan: The plan section outlining the proposed treatment and management plan should be comprehensive and clearly articulated. It can vary in length depending on the complexity of the case and the level of detail required. It may range from a paragraph to multiple paragraphs, addressing medications, therapies, referrals, follow-up appointments, and patient education.
If a nurse practitioner discovers an error in a previously written SOAP note, they should promptly notify the healthcare facility’s designated personnel responsible for managing documentation or medical records. Then document the error in an addendum or correction form, clearly stating the incorrect information and providing accurate details. Adhering to the facility’s policies and procedures, including seeking guidance from the legal department or compliance officers, ensures compliance with applicable laws and regulations. Using the incident as a learning opportunity, nurse practitioners should reflect on the error, identify its underlying cause, and implement strategies to prevent similar errors, promoting professional growth and maintaining a high standard of documentation integrity.
Key Points
Utilizing a Nurse Practitioner SOAP Note Example empowers nurse practitioners to maintain standardized and comprehensive documentation. The structured format of the SOAP note ensures that all essential components are captured, facilitating effective communication among healthcare professionals and supporting continuity of care. By referencing examples, nurse practitioners can enhance their documentation proficiency, streamline their workflow, and provide accurate and comprehensive records of patient encounters. Ultimately, SOAP note examples contribute to improved patient outcomes, interdisciplinary collaboration, and the delivery of high-quality care.