As healthcare professionals, maintaining accurate and detailed patient records is of paramount importance. One critical aspect of this documentation is the nursing SOAP note. These notes serve as a comprehensive record of a patient’s care, allowing healthcare providers to track progress, communicate important information, and ensure legal protection. By using a standardized template to create nursing SOAP notes, medical professionals can save time and ensure consistency in their documentation.
What Is a Nursing Soap Note?
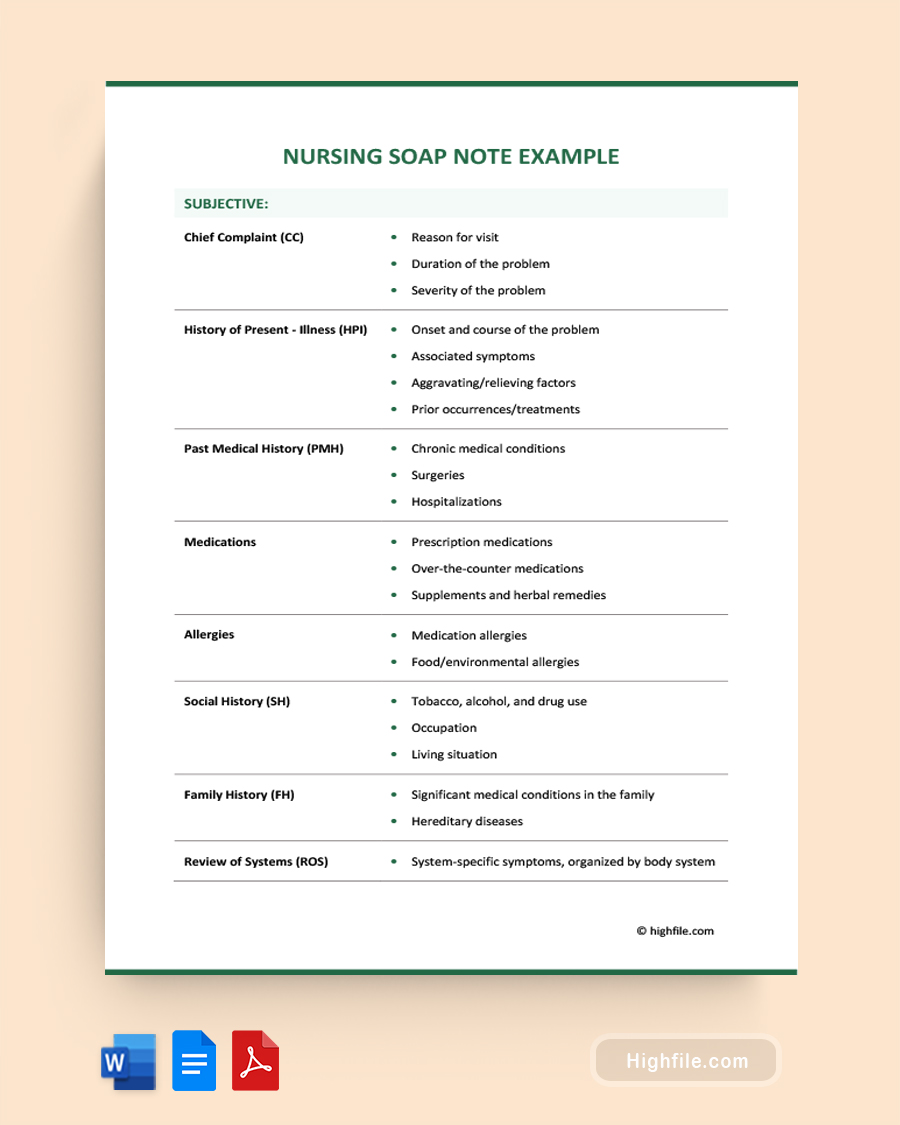
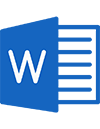
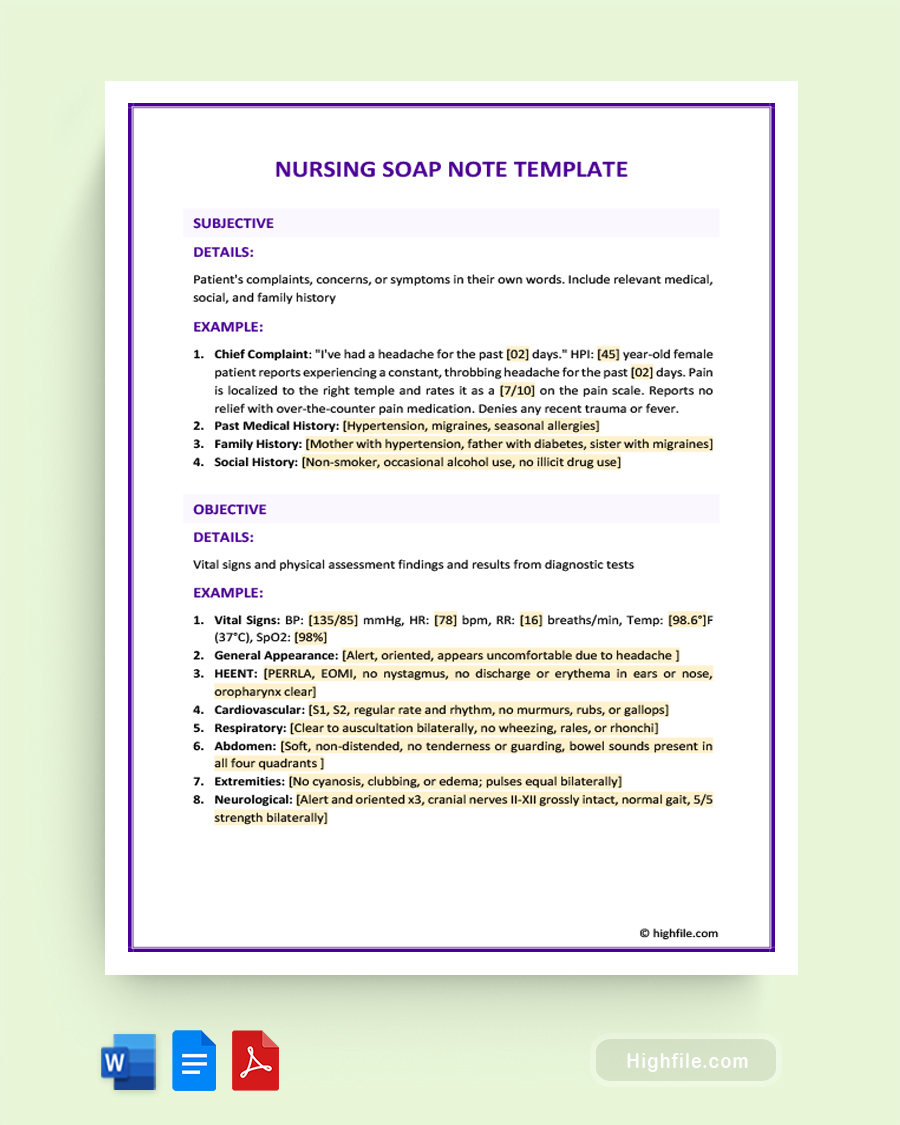
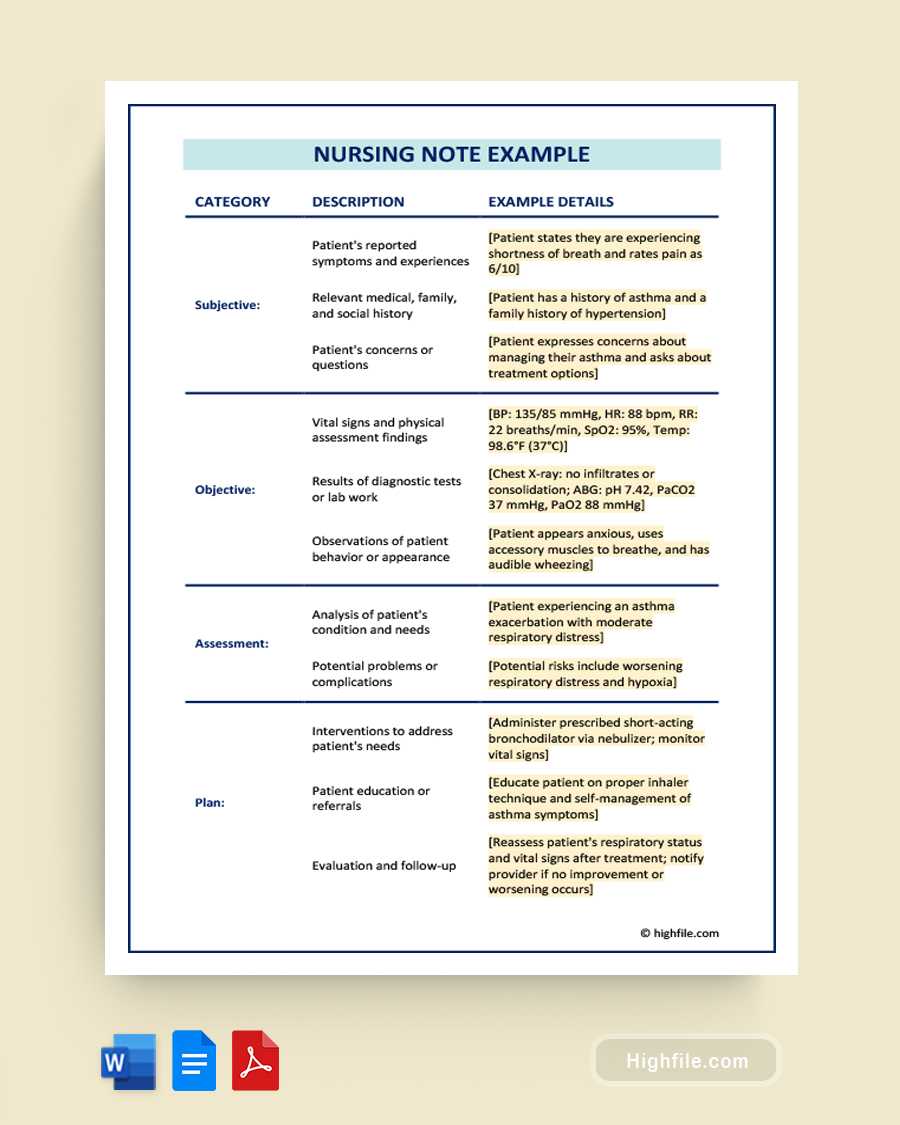
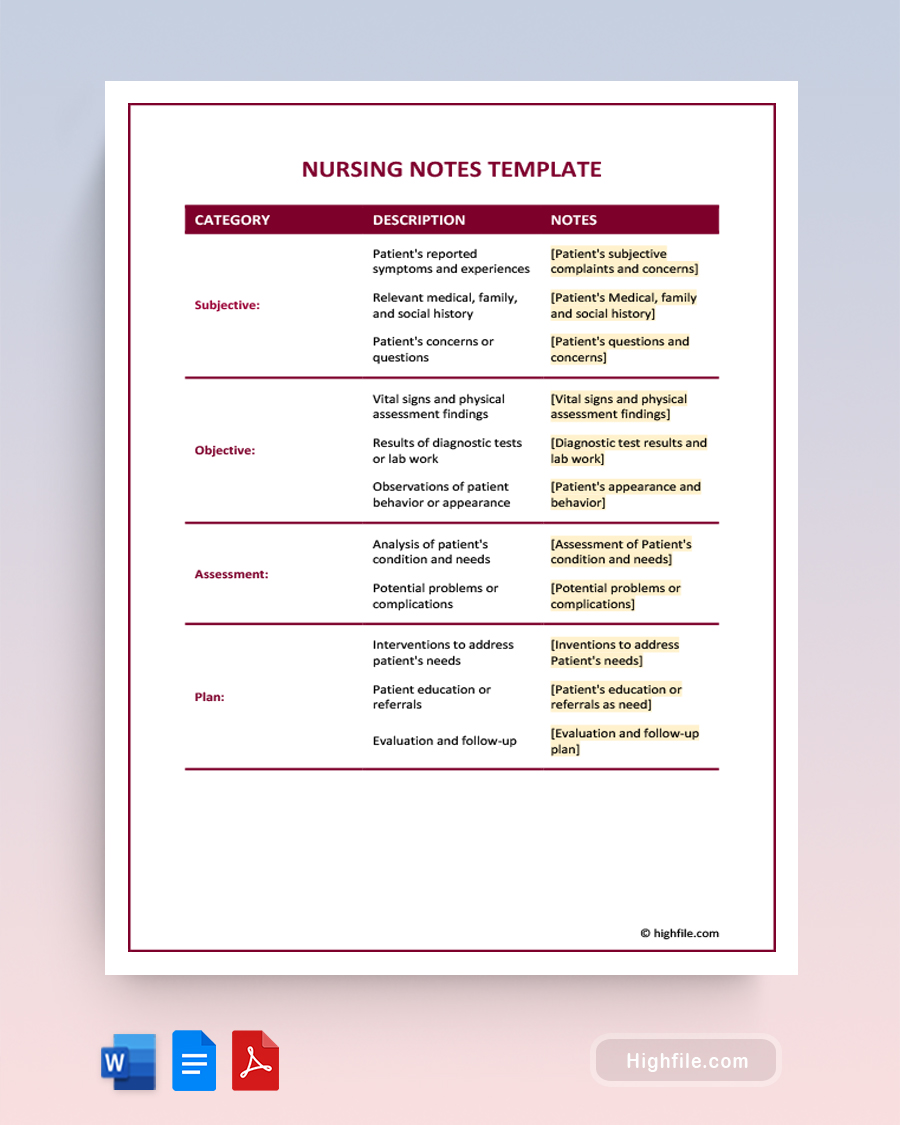
A nursing SOAP note is a documentation method healthcare professionals use to document a patient’s health status and care plan. The SOAP acronym stands for Subjective, Objective, Assessment, and Plan. The subjective section includes information about the patient’s symptoms, feelings, and concerns. The objective section includes data that can be measured, such as vital signs, lab results, and physical exam findings. The assessment section includes the healthcare provider’s professional judgment about the patient’s condition, diagnosis, and potential complications. The plan section includes interventions and treatments that will be initiated or continued, along with any follow-up care that may be needed. SOAP notes communicate crucial patient information among healthcare providers, track progress over time, and ensure continuity of care.
What is a Nursing Soap Note Example?
A nursing soap note documents a patient’s health status and care plan using the SOAP format (Subjective, Objective, Assessment, and Plan). Here’s an example of a nursing soap note for a patient:
- S: Patient complains of abdominal pain and nausea
- O: Vital signs stable, abdomen tender to palpation in upper right quadrant, no bowel sounds heard
- A: Suspected cholecystitis
- P: Administer IV fluids and pain medication, order ultrasound of gallbladder, consult with surgeon for possible cholecystectomy
- In this example, “S” refers to the subjective information provided by the patient, “O” refers to the objective information gathered by the nurse, “A” refers to the nurse’s assessment of the patient’s condition, and “P” refers to the nurse’s plan for care. This type of documentation helps to ensure that all healthcare providers have access to current and accurate information about the patient’s care.
Pro Tip: Although it is essential for you, as a medical provider, to remain objective, you can and should note the patient’s emotional state under the ‘subjective’ section. A patient’s mental state can impact their overall health, so sharing these insights can help your team.
How Can a Nursing Soap Note Example Help You?
A nursing SOAP note example can be helpful in many ways.
- Provides a template: A nursing SOAP note example can provide a framework for structuring your notes. This can help ensure that you are including all the necessary information and documenting it in a clear and organized way.
- Demonstrates proper documentation: A nursing SOAP note example can demonstrate how to document a patient’s health status and care plan properly. This can help you ensure that your notes are accurate, complete, and compliant with healthcare regulations.
- Provides reference material: A nursing SOAP note example can be a reference for future patient encounters. If you encounter a similar situation, refer to the example note to refresh your memory on how to document the encounter.
- Clinical reasoning: Examining well-crafted SOAP note examples can enhance clinical reasoning skills by demonstrating how to gather and interpret subjective and objective data, analyze the information, and derive appropriate conclusions.
- Preparation for EHR: Electronic Health Records (EHR) are commonly used in healthcare settings, and SOAP notes are often integrated into EHR systems. Reviewing SOAP note examples can help familiarize nurses with the structure and content required in electronic documentation, improving efficiency and accuracy when using EHR.
- Clarifies SOAP structure: SOAP notes follow a structured format (Subjective, Objective, Assessment, and Plan) to ensure organized and comprehensive documentation. Examples can clarify the expected content and sequencing of information in each section, enabling nurses to create well-structured SOAP notes.
- Promotes legal and ethical practice: SOAP note examples can highlight the importance of adhering to legal and ethical guidelines in documentation. They demonstrate the need for accurate and objective reporting, protecting patient privacy and confidentiality, and ensuring proper documentation of assessments, interventions, and treatment plans.
FAQs
Incorporating patient education into the Plan component of the SOAP note is an important aspect of nursing care. Here are a few steps you can take to ensure that patient education is included in the SOAP note:
ᐅ Identify the educational need: The first step in incorporating patient education into the Plan component of the SOAP note is to identify the patient’s educational need. This may include their diagnosis, treatment plan, or medication regimen information.
ᐅ Document the educational intervention: Once you have identified the educational need, document the educational intervention you plan to provide. This may include written materials, verbal instructions, or a demonstration of a specific skill.
ᐅ Include any necessary follow-up: Document any necessary follow-up that may be required to ensure that the patient understands the information provided. This may include scheduling a follow-up appointment, providing contact information for additional questions, or arranging a referral to another healthcare provider or specialist.
ᐅ Document the patient’s response: Finally, document the patient’s response to the educational intervention. This may include any questions or concerns the patient has and their reaction to the information provided. This documentation can help you track the patient’s progress and ensure they receive the education and support they need to manage their health effectively.
Here is an example of how you can incorporate patient education into the Plan component of a SOAP note:
P: The patient will receive written materials and verbal instructions on managing their diabetes. The patient will be referred to a dietician for further education on a diabetic diet. Follow-up will be scheduled in 2 weeks to assess the patient’s understanding of the information provided and to adjust the treatment plan as needed. The patient expressed understanding of the information provided and demonstrated the ability to self-administer insulin injections. The patient will be encouraged to contact the healthcare provider with questions or concerns.
S: Patient complains of pain in the right knee.
O: Knee slightly swollen, patient limping while walking.
A: Knee pain.
P: Administer pain medication.
Reasons why this is an ineffective example:
ᐅ Lack of detail: The subjective (S) section lacks specific information about the nature of the pain, its duration, aggravating or relieving factors, or any associated symptoms, which hinders a comprehensive understanding of the patient’s condition.
ᐅ Incomplete objective (O) assessment: The objective section merely mentions a swollen knee and the patient limping without providing essential details such as the degree of swelling, range of motion, or additional findings that could aid in a more accurate assessment.
ᐅ Superficial analysis (A): The assessment states “knee pain” without delving into potential causes, underlying conditions, or a more detailed diagnosis, leaving out crucial information that could guide further interventions.
ᐅ Vague treatment plan (P): The treatment plan suggests administering pain medication without specifying the medication type, dosage, frequency, or additional interventions or follow-up actions.
A comprehensive and well-written SOAP note should provide thorough subjective information, detailed objective observations, a comprehensive analysis, and a specific treatment plan considering individual patient needs and goals.
Key Points
Medical professionals use nursing SOAP notes to document patient care and progress and communicate important information between healthcare providers. Nursing SOAP notes provide legal protection, ensure continuity of care, and facilitate communication. Using a template to create nursing SOAP notes ensures consistency, helps you learn proper documentation skills, and saves time by providing a framework that is accessible to all team members.