Nursing SOAP notes are critical to healthcare because they provide a concise and structured method for nurses to document patient care. The acronym SOAP stands for subjective, objective, assessment, and plan, and these four elements form the basis of the note. By using a template to create these crucial documents, you can efficiently and effectively create a streamlined system for writing the notes, making it easier for your whole team to understand and share the information.
What Is a Nursing Soap Note?
A Nursing Soap Note is a medical documentation tool nurses use to record and monitor patient care. “SOAP” stands for Subjective, Objective, Assessment, and Plan, which are the four sections of the note. In the note, nurses document their observations of a patient’s condition, analyze the information, and develop a care plan to improve their health.
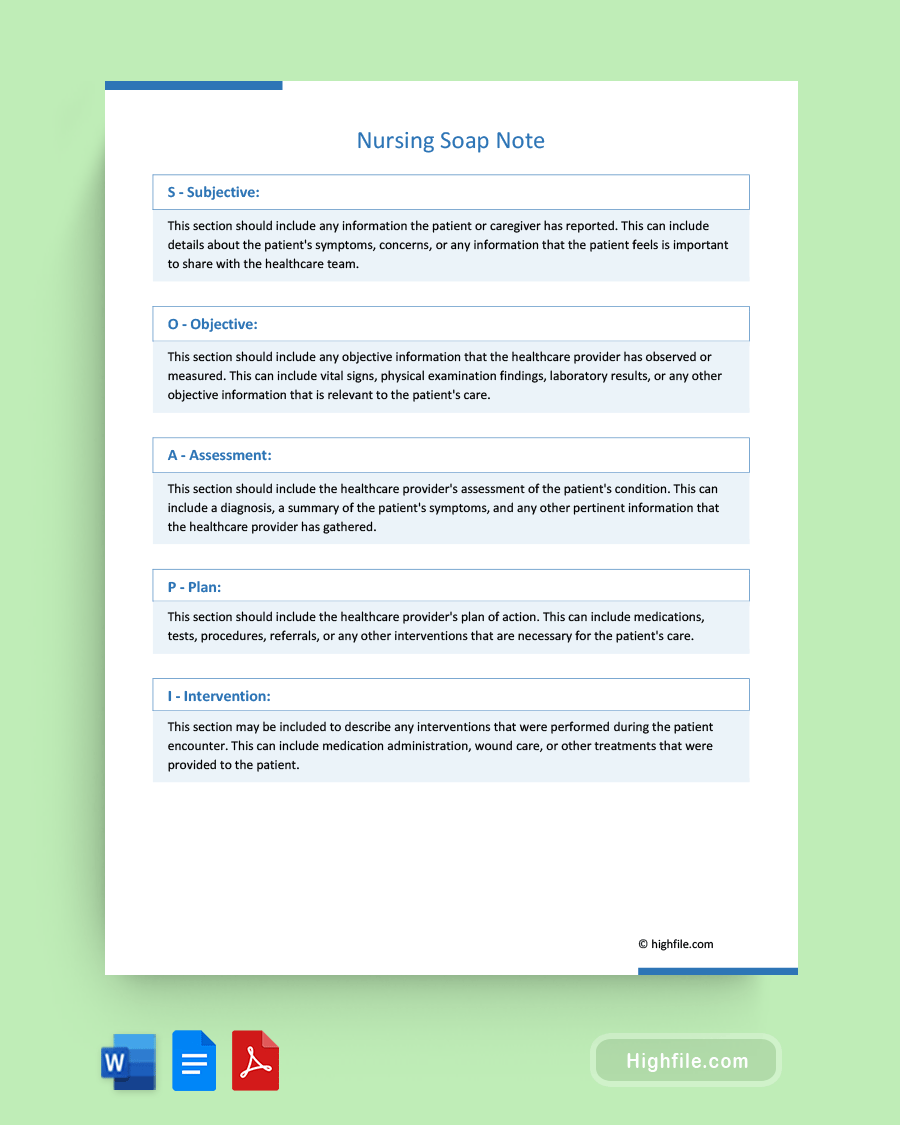
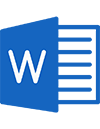
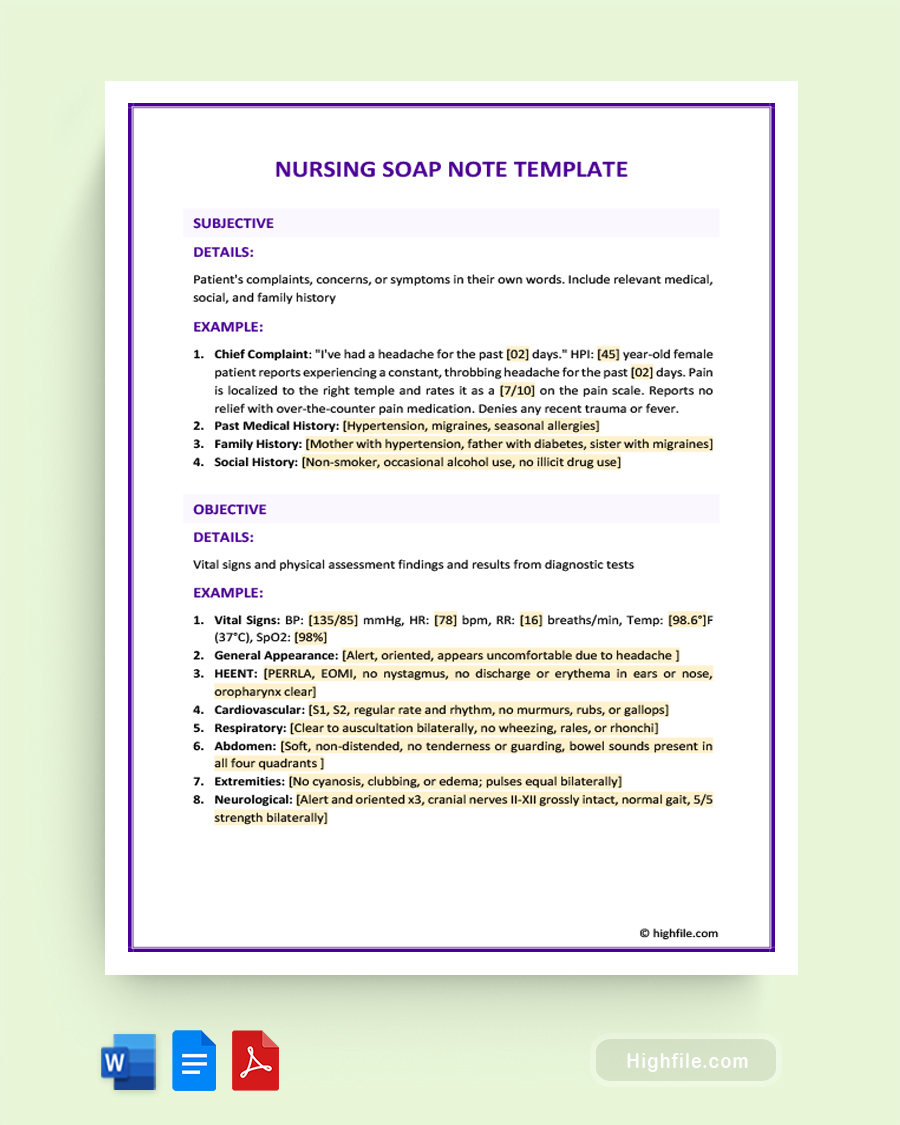
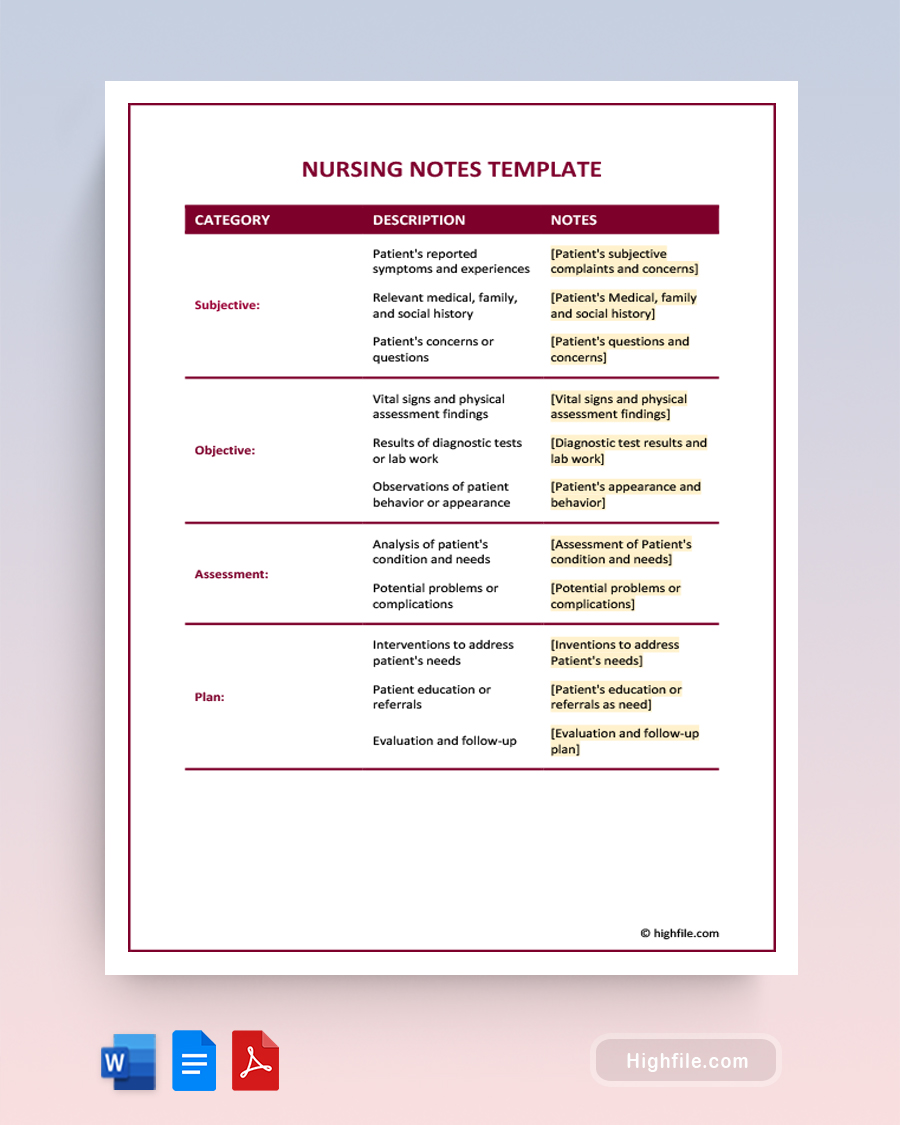
The subjective section includes information about the patient’s symptoms, concerns, and any information the patient or family members provide. The objective section contains data obtained through observation, examination, and diagnostic tests, such as vital signs, laboratory results, and physical findings. The assessment section includes the nurse’s clinical impression or diagnosis based on subjective and objective data. Finally, the plan section outlines the nursing interventions and treatment plan.
Fun Fact: The acronym “SOAP” for Nursing SOAP Note was coined by Dr. Lawrence Weed in the 1960s, who developed the format. Dr. Weed’s wife, a medical librarian, suggested the acronym to make it more memorable. Today, the SOAP format is widely accepted for organizing patient notes and is used globally to document care and improve communication among healthcare teams.
Importance of Nursing Soap Note in Patient Care
The nursing SOAP note is important in patient care as it provides a structured and organized way for nurses to document patient information, track progress, and communicate with other healthcare professionals. It helps to ensure that all relevant information about the patient’s condition, care plan, and progress is recorded accurately and completely. It also allows for continuity of care as different nurses or healthcare providers can easily review the patient’s history and progress notes.
The benefits of nursing soap notes in patient care include:
- Improved communication: Nursing soap notes provide a standardized way for healthcare professionals to communicate about a patient’s care. This ensures that all healthcare team members are on the same page and can provide coordinated care.
- Better patient outcomes: By keeping detailed records of a patient’s care, nursing soap notes can help healthcare professionals identify trends and patterns in a patient’s health status. Doing this can lead to more effective treatment plans and better patient outcomes.
- Legal protection: Nursing soap notes can serve as legal documentation of a patient’s care, which can be important in the event of a malpractice lawsuit or other legal action.
- Improved quality of care: Nursing soap notes can help healthcare professionals identify areas where they can improve their quality of care. Healthcare professionals can continually improve their practices by tracking patient outcomes and evaluating the effectiveness of different interventions.
- Efficient use of time: Nursing soap notes can help healthcare professionals be more efficient with their time. Healthcare professionals can quickly review a patient’s history and determine the appropriate course of action using a standardized format for recording patient information.
Pro Tip: While Nursing SOAP Notes are crucial for documenting patient care, other means of communication should exist among healthcare providers. Other forms of communication, like emails or face-to-face meetings, should always supplement SOAP notes. Good communication among healthcare providers is crucial, as it can prevent mistakes, reduce duplicated work, and ultimately lead to better patient outcomes.
Essential Elements of a Nursing Soap Note
- Form Title and Date- Not all SOAP notes use a specific title, so it’s best to use the standards set forth by your specific hospital or medical care facility. Add the date to avoid confusion.
- Subjective- Subjective data includes patient concerns and other non-fact-based information that may impact treatment.
- Objective- Objective information should consist of fact-based data such as lab results.
- Physical Exam- This category is for physical examinations such as checking the lungs, heart, or abdomen.
- Assessment- The Assessment can include a diagnosis, if relevant, or other assessment notes on the patient’s condition.
- Plan- The plan should include prescriptions, referrals, treatments, and other interventions that have yet to be performed.
- Intervention- If any interventions were performed during the patient intervention, such as giving medication, they should be noted here.
- Response- Include notes on how the patient responded to the intervention if relevant.
- Education- Keeping notes on what education has been given to the subject can help avoid unnecessary redundancies and help ensure the patient understands vital issues like their paperwork or aftercare requirements.
- Follow-Up- Add any helpful information about the necessary follow-ups, like additional appointments.
Guidelines for Writing a Nursing Soap Note
Here are some general guidelines for writing a nursing SOAP note. Following these guidelines, you can create clear and concise SOAP notes that communicate important patient information with other healthcare providers.
- Use a standardized format: The SOAP note format provides a clear and structured way to organize patient information. It includes four sections: subjective, objective, assessment, and plan. Use these headings to separate and organize the information clearly.
- Be concise: SOAP notes should be brief and to the point. Use only essential information and avoid including unnecessary details.
- Use objective language: Use clear and accurate language to describe the patient’s condition and avoid using subjective terms like “good” or “bad.”
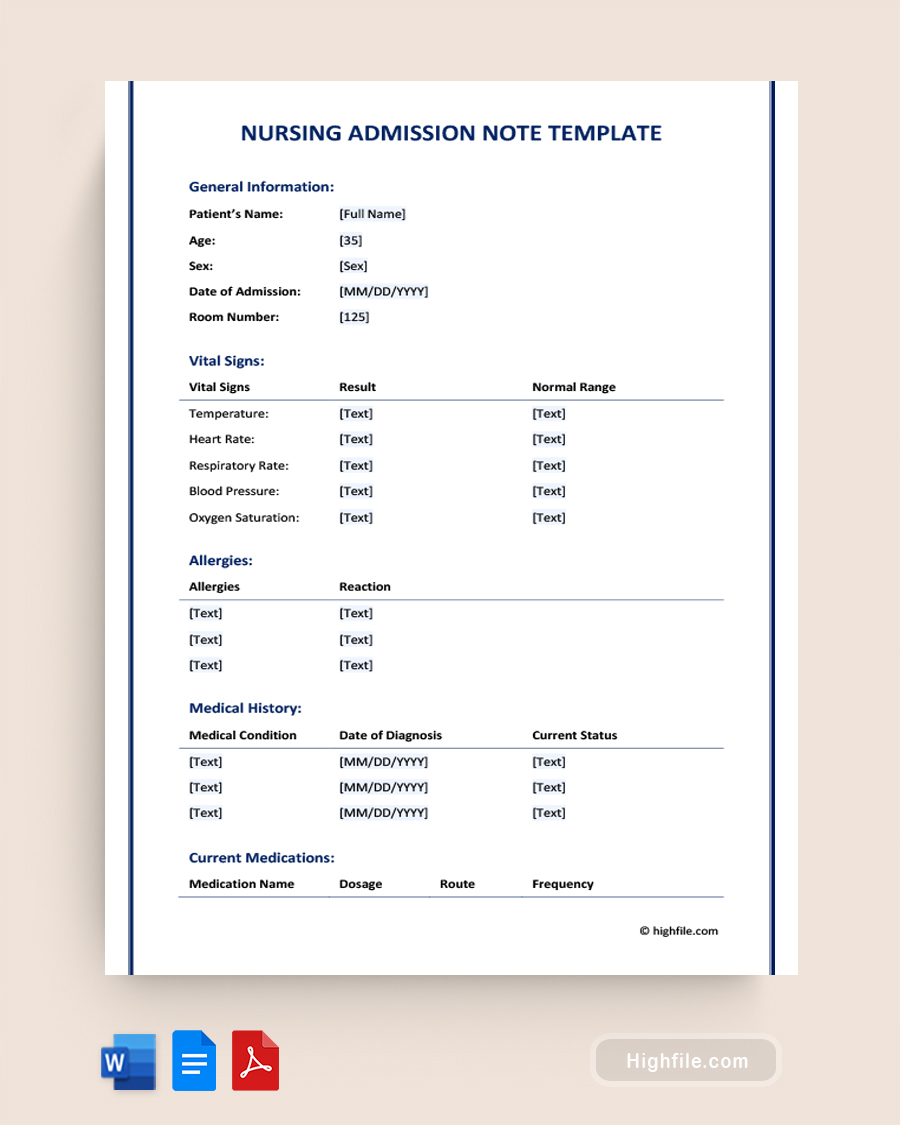
- Include relevant details: Include all relevant information about the patient, including vital signs, medications, laboratory results, and any pertinent medical history.
- Be specific: Be specific when describing the patient’s condition and any nursing interventions that have been implemented. Include details such as the time, date, and frequency of interventions.
- Follow the nursing process: Use the nursing process as a guide to assess, diagnose, plan, implement, and evaluate the patient’s care. Use the SOAP note to document each step of the process.
- Document any changes: Document any changes in the patient’s condition or response to treatment. Doing this will help you to track the patient’s progress and adjust the care plan as necessary.
- Avoid assumptions: Avoid making assumptions about the patient’s condition or behavior. Stick to the facts and avoid making subjective judgments.
- Review and revise: Review your SOAP notes regularly to ensure they are accurate and up-to-date. Revise them to reflect changes in the patient’s condition or care plan.
Pro Tip: Take a structured approach. Structured documentation methods, such as the DAR format, promote consistent and organized documentation, facilitate communication and collaboration among healthcare providers, identify patterns and trends in a patient’s condition, and ultimately improve patient care quality. By using a standardized format, healthcare providers can capture all necessary information in a clear and concise manner, leading to more efficient and coordinated care.
How Can Nursing Soap Note Examples Help You?
Nursing soap notes provide a systematic and organized way to record patient care and treatment, making it easier for healthcare professionals to communicate and coordinate. However, creating accurate and effective nursing soap notes can be challenging, especially for new nurses or those needing more documentation experience. Nursing soap note examples can be a valuable resource in such situations, helping nurses understand the format, content, and structure of an effective nursing soap note. This way, they can learn to create high-quality notes that meet legal and ethical standards. Here are more ways Nursing SOAP Note Examples are helpful:
- Understanding structure and format: Reviewing examples can help you understand the note’s structure and layout, aiding you in organizing your own notes.
- Identifying important details: Examples can help you recognize crucial information, like vital signs and lab results, to ensure nothing essential is left out.
- Improving documentation skills: Examining examples can improve your note-taking abilities, helping you write clear, concise, and specific notes and enhancing communication and care coordination.
- Learning from healthcare providers: SOAP note examples provide insights into others’ approaches to care and documentation, enabling you to learn from their experiences and adopt best practices.
- Adapting to EHRs: Examples can assist you in adapting to electronic health records, improving the accuracy and completeness of your notes, and streamlining your documentation process.
- Legal and regulatory compliance: Nursing SOAP note examples can help you understand the legal and regulatory requirements for documentation, such as HIPAA regulations, and how to comply with them. This can help to prevent legal and ethical issues that may arise due to inadequate documentation.
- Facilitating interprofessional collaboration: SOAP note examples can facilitate interprofessional collaboration by providing a clear and concise summary of the patient’s condition and care plan. Using examples and a standardized format can improve communication among healthcare providers, leading to more effective and coordinated patient care.
Legal and Ethical Implications of Nursing Soap Note
When it comes to documenting patient care, nursing soap notes play a critical role in ensuring accurate and comprehensive records. However, along with their importance comes a responsibility to ensure that they are created and maintained in compliance with legal and ethical standards. Failure to do so can have serious consequences for the patient and the healthcare provider. Below, we will explore nursing soap notes’ legal and ethical implications to help healthcare professionals better understand their responsibilities and obligations.
Legal Implications of Nursing Soap Note
- Failure to document accurately can result in legal action against the healthcare provider.
- Patients can request access to their medical records, including Nursing Soap Notes, under HIPAA and other privacy laws.
- Incomplete or inaccurate documentation can result in insurance denials and delays in payment.
- Non-compliance with documentation standards can lead to legal consequences and malpractice suits.
- Failure to obtain patient consent or share information with unauthorized parties can result in violations of privacy and confidentiality laws.
Ethical Implications of Nursing Soap Note
- Maintaining patient confidentiality and privacy is crucial when documenting sensitive health information.
- Ethical concerns may arise when sharing information with third parties or using the information for research purposes without obtaining proper consent.
- Nurses must ensure they document objectively and accurately to avoid ethical concerns related to bias or misrepresentation. Failure to document appropriately can be viewed as a violation of professional standards and codes of ethics.
- Inaccurate or incomplete documentation can result in ethical dilemmas and conflicts between healthcare professionals and patients.
- Using subjective language or biased documentation can result in discrimination or unequal treatment of patients.
FAQs
Here are answers to the most frequently asked questions about Nursing Soap Notes.
It is generally recommended to refrain from using abbreviations and medical jargon in nursing soap notes, as they can be difficult for other healthcare professionals to understand. Unfortunately, doing this can lead to misinterpretation or errors in patient care. Instead, it is best to use clear, concise language and define any technical terms or abbreviations used.
Nursing SOAP notes can be used to document telehealth encounters. The notes should include the same information as in-person encounters, such as the patient’s current symptoms, vital signs, medications, and any interventions or treatments provided during the telehealth session. The SOAP note should also include any relevant information discussed during the telehealth encounter, such as the patient’s concerns, questions, and follow-up care instructions.
To ensure that your Nursing Soap Note is compliant with privacy and data protection laws, you should follow these steps:
ᐅ Obtain the patient’s consent: Before documenting patient information, obtain their written consent to use and disclose their information for treatment purposes.
ᐅ Keep the information confidential: Store the patient’s information in a secure location and limit access to only those individuals who need to know the information for treatment purposes.
ᐅ Use de-identified information: When possible, use de-identified information in the Nursing Soap Note, such as initials or unique identifiers, to minimize the risk of exposing sensitive patient information.
ᐅ Follow HIPAA guidelines: Familiarize yourself with the HIPAA guidelines and ensure that your documentation practices comply with these guidelines.
ᐅ Keep up-to-date with privacy laws: Stay up-to-date with any privacy and data protection laws changes, and adjust your documentation practices as necessary.
Nursing Soap Notes are considered part of a patient’s medical record and are subject to privacy laws such as HIPAA in the United States. This means sharing the note with patients or their families would require explicit consent and compliance with relevant privacy laws. However, in some cases, healthcare providers may share certain information from the note with patients or their family members to facilitate their care and treatment. It’s essential to consult with your healthcare organization’s policies and legal counsel to ensure that any information sharing is done in compliance with relevant laws and regulations.
Nursing Soap Notes can be used to document the use of complementary and alternative therapies. It is crucial to accurately record all treatments and therapies provided to the patient to ensure that the patient receives appropriate and safe care. Additionally, it is important to use clear and concise language to document any complementary or alternative therapies or treatments and avoid making unsubstantiated claims about their effectiveness or safety.
Key Points
By using SOAP notes, nurses can communicate effectively with other healthcare providers about the patient’s condition and the care that has been provided. This information is critical to ensuring continuity of care, as it allows for a clear record of the patient’s progress and any changes in their condition. SOAP notes also help nurses identify gaps in the patient’s care and monitor their response to treatment. In addition, they can be used to track and evaluate the effectiveness of nursing interventions, identify potential complications, and make adjustments to the care plan as necessary.